My A-Z of Preparing for baby (Part 2; N-Z)
(adjective) of or for babies that were born recently.
Neonatal Unit: A neonatal intensive care unit (NICU), is an intensive care unit (ICU) specialising in the care of ill or premature new-born infants.
Units are a part of hospitals which provide care for babies who are born prematurely (before 37 weeks’ gestation), with a medical condition which needs treatment, or at a low birthweight. Over 100,000 babies are born premature or sick and needing neonatal care in the UK each year. That is one in seven babies, or around 300 babies every day.
There are different ways of describing a premature birth.
Ÿ Term = A baby that has spent at least 37 weeks inside the womb (gestation)
Ÿ Preterm = A baby born before 37 weeks’ gestation
Ÿ Moderate to late preterm = A baby born between 32- and 37-weeks’ gestation
Ÿ Very preterm = A baby born between 28- and 32-weeks’ gestation
Ÿ Extremely preterm = A baby born at or before 28 weeks’ gestation
There are different ways of describing a low birthweight baby.
Ÿ Low birth weight = Born weighing less than 2500g (5lbs)
Ÿ Very low birth weight = Born weighing less than 1500g (3lbs)
Ÿ Extremely low birth weight = Born weighing less than 1000g (2lbs)
Birth is already an emotionally & physically exhausting process & whether or not you know that your baby will need to spend time in NICU, it can still be an anxious & confusing time.
You will naturally want to spend as much time as possible with your baby(ies) - but please remember to look after yourself. Some mothers & other parents of NICU babies describe feeling "lost & forgotten about". The Neonatal Nurses are there to care for your baby & it can be all too easy to forget that the birthing parent is recovering & needs support & to be cared for too, especially once you have been discharged from hospital care yourself.
Keep reaching out to those around you & talk about how you are feeling.
Food parcels, comfort breaks, phone calls to check in on them & general support will be important during this time (made even more difficult during the pandemic & hospital visiting restrictions.)
Human milk &/or donor human milk can be particularly important for sick, low birth weight &/or premature babies. Something practical you can do to support your baby is to express your colostrum & then milk to help your baby to grow & fight off infections. The hospital will be able to give you access to a hospital grade pump, storage & they will even refrigerate/freeze your milk for baby. (see Part 1 of this blog & C for Colostrum & I for Infant Feeding for further information)
You may also wish to investigate the benefits of kangaroo care to support your neonates development too. Read more on this subject on the following links. Le Leche League, National Institute for Health Research & Hand to Hold.
Further sources of information & support for parents of NICU babies include.
Bliss, Tommys, NHS & Support 4 NICU Parents.
It may be a while before you feel able to fully open up, be honest & talk about your birth &/or nicu experiences, & that is understandable - but please don't let that stop you from seeking the support & understanding that you, your partner & your family may need & benefit from.
O is for Obstetrician
(noun) a doctor with special training in how to care for pregnant women & other birthing people & help in the birth of babies.
As I mentioned in Part 1 – M is for Midwife, in the most part, you will be "booked in", by a midwife & they will continue to provide most, if not all of your care during pregnancy, birth & postnatally.
However, if your pregnancy is deemed "high-risk", then you will be referred for consultant led care. About 35% of births are undertaken by an obstetrician, usually for more complex cases or if the baby becomes distressed during labour. Their work includes:
- using instruments to assist delivery – including forceps or a ventouse (vacuum-assisted delivery)
- performing caesarean sections, either as a planned or emergency procedure
- antenatal clinics
Why I might be considered, "high-risk"?
* You have an acute or chronic medical condition which may affect your pregnancy &/or birth E.g. - diabetes, a heart condition, epilepsy, crohn’s, etc… or a physical disability
* Your baby is
identified as having a known medical condition or complication
* You've had a
previous pregnancy complication
* You develop a
pregnancy related condition that requires extra treatment or support. E.g., gestational
diabetes, obstetric cholestasis or preeclampsia
* You conceived
via IVF
* Your BMI is considered
too high or too low
* You are
considered an "older" or "younger" mother or gestational parent
* Your baby is
measuring "big" or "small" for gestational age
* Your baby has a breech or transverse presentation after 35wks gestation
As you can see
- that list seems to fall into 2 categories:
i) an actual
medical issue that needs more careful consideration, care & support
ii) something which has been deemed "risky" because you or your pregnancy falls outside of medicines pre-determined acceptable boundaries.
People are all
different - So understandably, pregnancy & birth will also look different
in different circumstances too. Your age, size, gender, sexuality, ethnicity, disability,
or ability should not pre-determine the way you are treated or the autonomy you
are granted just because you are pregnant.
Whatever your circumstances are, YOU do the "allowing", the healthcare professionals cannot do anything without your explicit consent! You can request or decline any test, treatment, care plan, intervention, examination, etc... as you see fit. It is your body, your birth, your baby – so step into your own power, speak up & have your say. Any Obstetrician worth their salt, will be more than happy to support a woman or other birthing person, who has done their research & wants to take charge of ensuring a positive birth experience, in a safe & caring environment - not, "just" a healthy baby at the end of a traumatic experience.
(noun) the temporary organ that feeds a foetus (e.g., the developing baby) inside the womb
The placenta is an organ that develops in your uterus during pregnancy. This structure provides oxygen and nutrients to your growing baby and removes waste products from your baby's blood. The placenta attaches to the wall of your uterus, and your baby's umbilical cord comes from it, attaching baby to you.
As mentioned in the post, "L is for labour", the placenta is born after baby, in the 3rd stage of labour. At birth up to a 3rd of baby's blood is still inside the placenta. Half of that blood is transfused into baby by 1min of age & by 3mins, more than 90% of the transfusion will be complete. Therefore, I would recommend looking into delayed or optimal cord clamping. Read more here.
Cord Ties: Usually an embroidery, knitted or crocheted "tie", wrapped & tied around the cord instead of the plastic clamp midwives usually use to seal baby's umbilical cord closed when it is cut. These are a softer, more natural/eco-friendly alternative & can be purchased from places like Etsy or you can even make your own!
Check out – Heartstrings umbilical cord ties to see some truly beautiful creations 😍 Or checkout Pintrest for instructions on making your own.
Follow this link to see a video by Independent Midwife Deborah Neiger on how to tie a cord tie.
So, what now for the placenta?
Well firstly, if you are interested - ask your midwife to show it too you & talk you through this amazing organ! It needs to be checked over postnatally to ensure it is complete etc… & they are more than happy to do this with you. The hospital can then dispose of it for you - OR - you might decide to keep it...!?
There are various cultures around the world 🌎 that have special rituals involving the placenta, for example - in the Maori culture the placenta is often buried (given back to the land) in a place with ancestral connection. It is also buried in Cambodia, Nigeria & Malaysia too. However, in Western society it is becoming increasingly popular to consume your placenta in some form. This can include encapsulation, homeopathy, essences & tinctures as well as blending pieces of raw placenta into smoothies to drink in the postpartum period or even frying it up to eat.
Placenta remedies have many benefits for the postnatal woman or other gestational parent, including - balancing hormones, lower rates of postnatal depression, increased milk supply & increased energy levels to name a few...
The Placenta Remedies Network is a not-for-profit UK based international network of Placenta Remedy Specialists, dedicated to supporting new families wishing to benefit from their placentas to boost their natural postnatal recovery. Placenta Remedy Specialist members are trained by accredited providers, IPEN or Prism Placenta & inspected by the Food Standards Agency (FSA), practitioners must register with their local councils Environmental Health department to be graded for hygiene (just like all restaurants) too.
Locally, as a Doula, I am blessed to know personally & often work with two placenta remedy specialists -
Kimberley at Placenta Mamas based in Fareham &
Caroline at The Placenta Cabin based in Bognor (Caroline is also a qualified nutritionist & homeopath)
So, if you want to talk to someone more experienced, don't hesitate to get in touch with either of these specialists or check out who your local specialist is at the PRN website.
Read more about the options for birthing your placenta here: Dr Sara Wickham & Aims
Q is for Questions
If you have
been following for a while, you'll know I'm a BIG advocate of informed decision
making 🤩
Researching, knowing & understanding pregnancy & birth options so you can make the right informed choices for YOU & YOUR baby.
Your Midwife &/or Obstetrician are there to answer your questions & make recommendations for your care based on their knowledge & understanding of pregnancy & birth - BUT - not, necessarily based on YOU, as an individual. Many women & other birthing people these days will be deemed, "high-risk". This could be due to age, physical disability, gender identity, size, medical, history, a previous caesarean birth or induction, a large or small baby, the list goes on... Unfortunately, because you've "ticked a box" ✅ somewhere in the system, this can influence the recommendations, care & options presented to you. This is why questions are so important!
Tools that can
help you:
✴ When being presented with information &/or recommendations by your Healthcare Provider, ask for their sources - so you can look them up & do further research for yourself
✴ Ask, Why?
& keep on asking why, until you get down to the bare bones of the
situation. If ultimately, the reason "why?", is - "because it is
hospital policy" or "that's just the way it is"... then, if it
doesn't sit well with you or you don't want it - you can decline
✴ Use the
B.R.A.I.N acronym to aid your decision making. This stands for -
B - Benefits.
What are the benefits of accepting this option AND the benefits of declining?
R - Risks. (or
chance) What are the risks of accepting this option AND benefits of declining?
A -
Alternatives. There will always be an alternative option - it just may not be
presented to you unless you ask!
I - Instincts.
What does your gut tell you? What feels right for you?
N - Nothing.
What if you do nothing? For 10mins? An hour? A day? Etc...
And do not
forget - you can always change your mind – at ANY point.
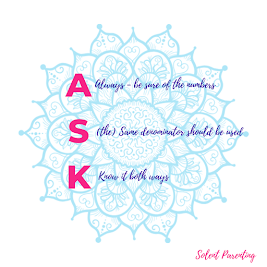
✴ Use the A.S.K
acronym.
A - Always be sure of the numbers being shared with you. Any risk factor should be expressed as an ABSOLUTE number, e.g. 6 people in 1000 & not as a relative risk, e.g. 6x as risky, or a percentage, e.g. a 60% increase - because those expressions are harder to understand & the evidence is that clinicians also get them wrong &/or misunderstand them too.
S - the Same
denominator should be used. e.g., 60 people in 1000, rather than 6 in 100 vs. 6
in 1000. Again, we are not known for being good at the Maths! The comparison
should be straight forward.
K - Know the
numbers both ways. e.g., if the chance of something happening is 5 in 100, then
the chance of it NOT happening is 95 in 100. Both sides of any
"chance" should be discussed.
✴ When visiting your midwife or obstetrician to ask questions & discuss your birth plans &/or care, I encourage you to make notes or even record your appointment. (This has been especially important during the pandemic, when pregnant people have been having to attend most appointments alone.) You are well within your rights to record what goes on at appointments - it makes it much easier to explain to your partner what was discussed & gives you an accurate reference point for double checking any information that was shared. The Informed Pregnancy, Birth & Beyond group that I help to facilitate shared a great post about this - linked here:
The BRAIN & ASK acronyms can help you talk to your health care professionals, midwives, consultant obstetricians,
when weighing up the pros & cons of situations. This is also another great
reason to consider having a Doula too! A doula can help you to navigate the
system, find unbiased, evidence-based information & most importantly support
YOU in your own choices, whatever they may be.
If you are
local (South East Hampshire/West Sussex) why not join the Informed Pregnancy,
Birth & Beyond Community group, over on Facebook too!? 😉
R is for
(postnatal) Recovery
(noun) the
process of becoming well again after an illness or injury...
the process of
being successful or normal again after problems...
the process of
getting something back...
Postnatal Recovery refers specifically to the rest, recuperation & recovery needed in the period after giving birth. Whether you have had a straightforward spontaneous vaginal birth, a long induction, or a planned or emergency caesarean birth, we all need time for rest & recuperation afterwards. The first six-twelve weeks postpartum are considered a “recovery” period. Your body has been stretched and stressed to the max, and it needs a chance to regroup.
A baby is not the only new person born at the end of a pregnancy - there will also be a new mama/papa/parent too, something that is often forgotten about. Everything is new - you are seeing the whole world through fresh eyes & it makes sense to take your time as you adjust to this new normal of, being a parent (whether it is for the first time or not). You will be tired (this may not change for quite some time, sorry...), overwhelmed, emotionally exhausted, your hormones will be all over the place, you are bleeding (yes, we bleed postnatally, regardless of what kind of birth we had, this is known as lochia & can last up to 6wks), you are producing colostrum & it can take 3-5days for your full milk to come in. You may have had tears or an episiotomy & stitches, you will feel swollen & uncomfortable. You may be taking painkillers or other medications recommended by your healthcare professionals, etc... & all on top of caring for a new baby who probably just wants to be held all the time - you are responsible for easing the womb to world transition for baby, as well as your own recovery during the fourth trimester period & selfcare & good nutrition can easily be forgotten about...
This is where us "Modern Westerners", have got things a little mixed up! Society seems to think we should get up & carry on regardless. That we should cope alone as new parents, bounce back & get on as if nothing has happened - no need to ask for help or support, that's showing weakness... BUT, we were NEVER meant to do this alone(!) & asking for help - planning for it, accepting it - is exactly what we should be doing, because we will feel better & be better parents for it!
There are some great resources available on Postnatal Recovery including:
From Postnatal Doula & Advocate, Sophie Messager
📚 Why Postnatal Recovery Matters, by Sophie Messager
📚 The
First 40 Days, (cookbook) by Heng Ou
📚 The
Postnatal Depletion Cure, by Dr Oscar Serrallach
📚 Mindful Mama, by Sophie Fletcher - this book includes some great mp3 tracks 🎧 to support you in the postnatal period too.
It is common
during your postnatal recovery to experience the "baby blues". Most
people during the initial days after childbirth, will experience feeling low,
sad, anxious, tired, overwhelmed & depressed... this is natural &
normal as we adapt & our hormones change & settle. However, if these
feelings do not improve & pass or, if they get worse, you may be
experiencing postnatal depression, postnatal anxiety, or postnatal rage. These
conditions are more commonly experienced by mums or birthing parents; however,
they can also affect partners & dads too. Please do not suffer in silence -
in these circumstances it is even more important to reach out for support.
You can find information & help on this from the following places: The Pandas Foundation (who have a local Hampshire group), Mark Williams at Fathers Mental Health, Solent Mind & be sure to speak to your Health Visitor or GP so you can get the help & support you deserve. Its Ok to Not Be Ok - but please reach out for support, you don't need to be alone.
S is for Skin-To-Skin
With people's body or parts of bodies touching directly, without clothing between them.
Skin-to-skin is essentially the act of placing a newly born infant directly onto the bare skin of their mother or gestational parent to enable the “golden hour” & hopefully initiate that first feed. In neonatal units it is often referred to as kangaroo care, helping parents to bond with their baby(ies) as well as supporting better physical & developmental outcomes for babies. We also know that skin-to-skin continues to be a valuable parenting tool for weeks, months & even for years to come.
It is a major
part of helping the baby to adjust to life outside the womb; the fourth trimester
concept. It is important for supporting the initiation of
breastfeeding/chestfeeding & for dads, partners, & other carers to
develop a close, loving relationship with their baby too.
* healthy
full-term babies carried skin-to-skin by their parents reap the same benefits
as premature babies
* use
skin-to-skin contact to soothe your baby at any time
* it can calm
& relax both parent & baby
* it helps to
regulate baby’s heart rate & breathing
* it’s great
for regulating temperature
* it enables
colonisation of the skin with the parents’ friendly bacteria, helping to
protect against infection
* it stimulates the release of oxytocin & other hormones important to breastfeeding / chestfeeding & parenting instincts
Studies into the benefits of skin-to-skin have shown that contact in the immediate postpartum period has a positive effect on the mother/parent-baby relationship at a year old when compared to pairs who were separated AND that contact of more than 20mins, resulted in an increased duration of exclusive breast / chest feeding!
Once you are home with baby many parents find that a sling can be a valuable parenting tool, helping to keep baby close & helping to ensure feelings of safety & security. A sling is also a great way to get some extra skin-to-skin contact in, something that baby & parents will all find beneficial.
Further sources & information can be found at the following links: Unicef, Carrying Matters, Le Leche League, Evidence Based Birth on skin-to-skin post caesarean birth.
T is for
Trimester
(noun) a period of three months, especially as a division of the duration of pregnancy.
The 1st trimester:
- Extreme fatigue
- Tender, swollen breasts. Nipples may protrude
- Nausea with or without throwing up (morning sickness)
- Cravings or aversion to certain foods
- Mood swings
- Constipation
- Frequent urination
- Headache
- Heartburn
- Weight gain or loss
The 2nd trimester:
Some women or other gestational people may find that their 1st trimester "symptoms" begin to ease, with the nausea & fatigue disappearing completely for some. You will notice more changes to your body including a baby bump, as your abdomen expands with the growing baby. By the end of the 2nd trimester, you will even begin to feel your baby move. Some other 2nd trimester changes -
- Back, abdomen, groin, or thigh aches and pains
- Stretch marks on your abdomen, breasts/chest, thighs, or buttocks
- Darkening of the skin around your nipples
- A line on the skin running from belly button to pubic hairline (linea nigra)
- Patches of darker skin, usually over the cheeks, forehead, nose, or upper lip. This is sometimes called the mask of pregnancy
- Numb or tingling hands (carpal tunnel syndrome)
- Itching on the abdomen, palms, and soles of the feet. (Call your midwife or doctor if you have nausea, loss of appetite, vomiting, yellowing of skin, or fatigue combined with itching. These can be signs of a liver problem.)
- Swelling of the ankles, fingers, and face. (If you notice any sudden or extreme swelling or if you gain a lot of weight quickly, call your midwife or doctor immediately. This could be a sign of a serious condition called preeclampsia.)
The final stage
of pregnancy. Discomforts that started in the second trimester will likely
continue, along with some new ones. As the baby grows and puts more pressure on
your internal organs, you may find you have difficulty breathing and must
urinate more frequently. This is normal and once you give birth these problems
should go away.
In this
trimester you may notice more physical changes including -
- Swelling of the ankles, fingers, and face. (As above - if you notice any sudden or extreme swelling or if you gain a lot of weight quickly, call your midwife or doctor right away. This could be a sign of a serious condition called preeclampsia.)
- Haemorrhoids
- Tender breasts/chest, & nipples which may leak a watery pre-milk called colostrum
- Your belly button may protrude
- The baby "dropping," or moving lower in your abdomen
- Contractions, which can be a sign of real or practice labour
Other symptoms you may notice in the third trimester include shortness of breath, heartburn, and difficulty sleeping. Your baby usually turns into a head-down position, ready for birth. In the last few weeks, they drop lower into your pelvis. Lastly your cervix begins to soften & efface ready for the process of labour to begin.
Pregnancy lasts 3 trimesters & then your baby will be born. However, you may have heard about the fourth trimester…!?
The 4th trimester:
This is the
12wk period immediately following birth. It is a time of great physical
and emotional change as your baby adjusts to being outside the womb, and you
adjust to your new life as a parent. Your body will be recovering from birth, you
will be adjusting emotionally, physically & practically to the ups &
downs of parenthood as well as for many, trying to establish breastfeeding/chestfeeding
& all of this on very little sleep.
Having the support of your extended family, friends or even a Doula can make a huge difference during this time - do not be afraid to ask for & accept help!
Further
Reading:
💻 NHS
📚 Let's Talk About Preparing for baby's birth, by Jackie Kietz
📚 Nurture: A Modern Guide to Pregnancy, Birth, Early Motherhood—and Trusting Yourself
and Your Body, by Erica Chidi Cohen
💻 NCT
📚 The
fourth trimester, by Kimberly Ann Johnson
U is for Ultrasound
scan
(noun) An Ultrasound Scan (also known as a Sonogram) is a procedure that uses high frequency sound waves to create an image of part of the inside of the body. Ultrasound Scans can be used during pregnancy to produce images of the baby in the womb.
You will be
offered at least two ultrasound scans during your pregnancy. If you have
experienced a previous loss, there are any issues with baby, you are carrying
multiples or you have certain medical issues that may put baby at risk, you
might be offered more scans. Like all the other tests and procedures,
you can choose whether to have the scans on offer or not.
Between week 11 and 13+6 you will be offered an ultrasound scan - for many expectant parents this is the first chance to see a glimpse of the tiny life inside you! Sometimes known as the dating scan, the sonographer (the person who scans you) will measure the size of your foetus & either confirm or adjust your EDD - "Estimated" due date based on these measurements. You will also be offered a nuchal translucency test to check the chance of the baby having Down's syndrome, Edward's Syndrome or Patau's Syndrome.
Your second ultrasound scan sometimes known as the, "20wk", "mid-pregnancy or "anomaly" scan, usually takes place between 18-21wks pregnant. It is offered to everyone - but you do not have to take it if you do not wish too. It is a medical examination & you will be asked for your consent for it to be carried out.
Please check with your hospital what their current guidance is around your partner & any others attending the scan with you. However, it is common for children to be discouraged or even prevented from attending.
Some pregnant women & other birthing people may be recommended by their midwife to have additional scan(s) during your 3rd trimester. This can often be to check on the baby’s growth & levels of amniotic fluid or for a presentation scan to check if baby is head down or not. These are "recommendations" - you can decline if you wish.
Although there is no evidence that scans are unsafe for your baby (unlike X-rays, which should be avoided in pregnancy), doctors cannot yet be sure that there is no risk at all to your baby. Because of this, it is not advisable to keep ‘looking’ unless your doctor or midwife needs to know more about your baby’s wellbeing. You can pay privately to have 3D scans (three-dimensional still pictures of your baby) or 4D scans (moving 3D images of your baby) but you should be aware that this involves extra unnecessary ultrasound scans.
Those expecting twins or multiples will be offered more scans, especially if they are sharing a placenta &/or amniotic sac as this may increase certain risks in pregnancy. You may be referred to an Obstetrician who has more experience of multiple births.
V is for
Vaginal Examinations
Some of the
reasons a Vaginal Examination may be offered:
·
On arriving at hospital during labour
·
To "establish" active labour has been reached
·
To assess favourability of the cervix before an induction
·
To administer the prostin, propess or dilapan rods
vaginally for induction
·
To check progress during labour
·
To find out how dilated you are
·
To confirm you are "fully dilated" (ready for
the 2nd stage)
·
To perform "Artificial Rupture of Membranes" (ARM)
·
To apply a foetal scalp electrode (FSE) to continuously
monitor baby
·
To perform foetal blood sampling
·
To exclude cord-prolapse after spontaneous rupture of
membranes, when the baby is positioned poorly
·
To access the presentation & position of baby
·
To perform a "stretch & sweep" antenatally
· Because it's policy
Often a woman or birthing person is asked to consent to a VE on arriving at hospital, the birthing unit or by a midwife attending a homebirth. They are then usually offered around every 4hrs throughout labour – but you can of course, decline! The midwife should always explain why an examination is being advised and what it will involve.
What are the
alternatives?
·
Watch & listen - it is usually possible to simply
observe a woman or birthing persons behaviour to assess how her labour is
progressing
·
The Purple line - a purplish line can be seen developing
from the anus up between the buttocks. For some it can be an indicator of
cervical dilation. E.g., length of line in cm's = no. of cm's dilated.
·
(Mexican) Hot legs - as labour progresses, blood flow
begins to be redirected to the uterus to help it do its work. This can mean
that the feet & calves begin to feel cold. When the colder part reaches
mid-calf, it is said to indicate you maybe 5cm dilated. This method is less
reliable if you have had pain relief & especially if you have had an
epidural. If you have been in a birth pool or shower, you will need to wait
approx. 20mins for the body to regulate.
Read more here:
💻 Aims,
Wonderfully
made Bellies & Babies.
W is for Waters Breaking (or - rupture of membranes)
As we discussed earlier in this series of posts, only a small percentage of women & other birthing people will experience their waters breaking before labour begins (approx. 15-20%) It is far more likely that they will release much later through the birthing process, possibly not until the 2nd stage & some babies are even born “en caul”, which means still inside their intact amniotic sac!
When your baby
is ready to be born, the amniotic sac ruptures & the fluid surrounding baby
comes out via your vagina. If your waters break naturally, you may feel a slow
trickle or a sudden gush of fluid that you cannot control or stop.
There is no need to be concerned about your waters breaking, but if you are less than 37wks pregnant, you should seek medical support as soon as possible, as you could be at risk of premature labour.
Sometimes, your midwife may offer to break your waters for you to induce or speed up your labour. This is known as "artificial rupture of membranes" (ARM) & as an intervention, should be given due consideration so you can make the right informed decision for you & your baby.
It should not hurt when your waters break OR if they are broken for you, as there are no pain receptors in the amniotic sac.
Many report
being "unsure" if their waters have broken or not... Often wondering
if they have wet themselves?
However, others report a very distinctive "Popping" sensation & a big gush of fluid. However amniotic fluid does not smell like urine! Put a sanitary/maternity pad (do not use a tampon) in your pants & monitor. Amniotic fluid is clear and a pale straw colour. Sometimes it is difficult to tell the difference between amniotic fluid & wee. The fluid may be a little bloodstained to begin with, this is normal.
Once your
waters have broken, your baby is at risk of infection and your midwife or
hospital/birth centre is likely to ask you to come into hospital to be checked.
Tell your
maternity unit immediately if:
·
the waters are smelly or coloured
·
you are losing blood
This could mean you and your baby need urgent attention.
If you are not sure if your waters have broken your Midwife may offer to check for you. This will mean you going into the maternity unit to be examined. The midwife, with your consent, will use a speculum to look at your cervix & may ask you to cough, to see if they can see fluid passing through.
Once your
waters have broken labour will usually begin naturally within 24hrs. However,
after 24hrs the chance of infection to baby begins to rise & you are likely
to be offered an induction. If you decline induction or it is unsuccessful,
your temperature will be monitored (if in hospital) or you will be asked to
monitor it yourself (if staying at home) every 4hrs, as a high temperature can
indicate signs of an infection. Otherwise, you can carry on as normal. Having a
bath or shower (plain water) is not thought to increase your risk of infection,
but having sex could, so you should avoid that.
Contact your
midwife if:
·
you develop a high temperature (around 37.5 degrees
Celsius)
·
you notice any change in the colour or smell of your
vaginal discharge
· you feel your baby's movements have changed or they are moving less. You should
continue to feel your baby move right up to the time you go into labour and during labour
If baby is head
down & engaged, it is most likely only your forewaters that escape, the
hind waters are blocked by baby's head. If labour progresses the hind waters
will be released in trickles &/or gushes as baby moves down & is born.
It is possible to have a hind waters leak & it reseal & stop leaking,
this can be more common if labour does not start straight away.
If the baby is high (not engaged) when your waters release, this can cause the umbilical cord to prolapse - when the cord comes in front of the baby’s head. This is an uncommon but serious situation & you will need immediate medical attention.
There is no need to stay at home as the end of your pregnancy approaches though - if you are concerned about your waters breaking away from home, you may find it helpful to try to be prepared by carrying sanitary/maternity pads with you & maybe some plastic sheeting/incontinence pads &/or towels, handy in your car.
Read more: Here,
Belly
Belly & Dr
Sara Wickham
X is for "Xciting!"
Discovering you are pregnant can certainly set you reeling! You may experience a whole host of emotions, thoughts & feelings, sometimes all at once & sometimes in waves as you contemplate what lies before you... & this is before you even begin to consider whether this was a planned pregnancy or not.
For many this is a, sometimes scary, but mostly exciting experience. You have made the decision to bring new life into this world & everyday closer you get to your birth the more excited you become to meet your baby & become a parent 🥰
Pregnancy can
be a joyous time of celebrations & firsts; first scan, first time hearing
the heartbeat, first movements felt, first craving, etc... & we are usually
able to share all of these with our partners &/or families. However - due
to Covid-19 & the maternity restrictions that followed, we have a whole
host of new parents who have been left feeling lost, unsupported, alone &
are unhappy with the loss of their pregnancy, birth & postnatal excitement
& stolen experiences. Hopefully, we are now coming through the pandemic
& maternity restrictions are being lifted – however, it is always wise to
remember that we are all different & ALL thoughts, feelings & emotions
are valid. Please seek support if you are struggling.
So many women & other birthing people still don't fully understand or appreciate quite what this phrase means...?
I know as a first-time expectant parent; I had no idea about my birth choices or rights... I wrote a "birth plan", but when things did not go "to plan", we did not question it... We did not push or ask why, when during labour I was told I couldn't use the birth pool. I didn't realise I could say "no" when they told me to move from kneeling over the back of the bed to being laid on my back (because it was more convenient to them) ...
As a Birth & Postnatal Doula I have lost count of the number of times I've heard, "Oh, but I didn't know I had a choice..." or "The Dr/Midwife said I would have to be induced/continuously monitored/on the bed/etc..."
Since birth was first moved into hospitals & began to be treated as a "medical condition" back in the 1950's, women & other birthing people have been being conditioned to put their trust in doctors & hospital policy & procedures over their own bodies & instincts. (However did the human race survive for so long... 😉)
There is a great quote from an American Birth Activist, January Harshe that goes…
"I don't care what kind of birth you have.... A homebirth a scheduled caesarean an epidural hospital birth or if you birth alone in the woods with baby deer.
I care that you had options, that you were supported in your choices & that you were respected!”
This really speaks to me & is how I strive to work with the expectant parents & families that choose me as their doula.
what to do, make choices for you or convince you to do anything YOU do not want... My role is to listen & understand what YOU want! To guide &/or signpost you to good evidence based information to discuss your options & support you to make the right informed choices for YOU & YOUR baby - whatever they may be - So that you feel calm, confident & well prepared going into labour, excited & supported to bring your baby into the world.
Birth is one of the biggest life transitions us humans experience - so let's reclaim our power & take charge of our birthing (& postnatal) experiences!
Birth Rights, Aims, Dr Sara Wickham & Evidence Based Birth are all excellent sources of evidence based information for helping you with your birth options 😉
Z is for Zzzzz...
(sleep) 😴
Hormonal changes in the 1st Trimester can leave you feeling tired, nauseous & emotional! Trying to eat healthily, resting when you can, ensuring you are well hydrated & accepting help or support from family, friends & colleagues can be really helpful - take care of yourself; you're growing another human after all.
As your
pregnancy progresses, you will also feel tired from the extra weight you are
carrying & your growing bump may prevent you from feeling comfortable in
bed or may mean having to get up & pee several times a night, meaning your
sleep is disturbed or unsettled.
The safest position to sleep in after 28wks is on your side - research suggests that sleeping on your back can increase the chance of stillbirth. You can support your bump &/or back with pillows & some women & other birthing people find that a pillow between the knees is also helpful.
Lots of pregnant people find they suffer from pregnancy insomnia. As difficult as this is to cope with, it will not harm your baby.
Things that
might help:
🎧 relaxation
- there are specific pregnancy relaxation classes available in most areas, such
as those from The Birth Tribe
Midwife as well as apps & you-tube videos. Check out your local antenatal
providers too, as many classes such as The Daisy Foundation Birthing classes also
include relaxation
🧘 yoga
- always ensure that the instructor has the correct training & insurances
to teach pregnancy yoga. This is not only a great way to relax, but also to
help you prepare physically, mentally & emotionally for your birth.
👃 aromatherapy
- this could be as simple as diffusing essential oils at home or booking an
aromatherapy massage or some reflexology 🦶 - again, always check the
practitioners credentials. See the local
support tab of my website for recommendations.
☕ A warm drink
- milk, cocoa, or herbal tea such as camomile are all said to have soothing
properties which can help you relax & aid sleep.
😴
Napping in the daytime &/or getting an early night
💻📱Reducing
the amount of screen time/blue light we are exposed too (a difficult one, I know).
If lack of sleep is bothering you, please talk to someone, a Midwife or Doctor or even just a friend.
Labour itself can be long (especially the early stage, before "active" labour begins) & tiring - mentally, physically & emotionally, so ensuring you have a trusted team around you to support & care for you will be helpful - whether that is your partner, sister, mum, friend, doula or whoever you choose. Do not forget that this support network can continue through into your postnatal period & even if you did not have a Birth Doula you could still have a Postnatal Doula to support your transition to parenthood. Part of that care can include support with family sleep - safe bedsharing &/or co-sleeping, watching baby so you can nap or shower 🚿, ensuring you rest, eat well & drink plenty which will all help you to navigate those early days of parenting, so you don't need to feel like you're running on adrenaline & cold tea...
It is worth
considering your sleeping arrangements before baby arrives, so you can make the
right informed choices for your family & so that if things change after
baby is born, you have the knowledge, support & confidence to make changes.
Current
recommendations are that baby sleeps in the same room as their primary caregiver
for ALL sleeps (ideally within arm’s reach) for the first 6 months of life, to
help reduce the chance of SIDS (Sudden Infant Death Syndrome) This could be in
a Moses basket, cot, crib, bedside cot or even in the family bed.
Basis Baby sleep Info Source are an excellent source of good evidence based information on normal infant sleep & safe sleep however you choose to sleep your baby. They also have an easy-to-use App you can download too.
For those who choose to breastfeed/chestfeed you may wish to consider a bedside cot or bedsharing, as this can help maximise the amount & quality of sleep you will all get as well as being safer for breast/chestfed babies.
Of course, not all of baby's sleep will take place in a cot or bed... many baby's (new-borns especially) love to contact nap with their caregivers & slings can also be a wonderful parenting tool to enable you to meet baby's needs as well as your own - you can read more on this subject from Dr Rosie Knowles at Carrying Matters here & here & from BASIS here.
Here are some
other reliable sources of sleep information:
* Lyndsey Hookway has written a fabulous, accessible book for parents called "Let's Talk
About Your New Families Sleep" & her website is also a valuable resource
Locally we are
blessed with a few Holistic Sleep Coaches (trained by Lyndsey Hookway &/or
Babyem) these practitioners look at the bigger picture & help support you
to better understand the sleep needs of your whole family. If this is something
that interests, you check out the local support tab (as above)



Comments
Post a Comment